Personalized Care Focused on Lifestyle Factors May Decrease AFib Risk for Individuals
Atrial fibrillation (AFib) is a common type of arrhythmia, affecting over individuals worldwide. Alongside well-known risk factors like physical activity, diabetes, obesity, and smoking, several other factors play a role in AFib development and management.
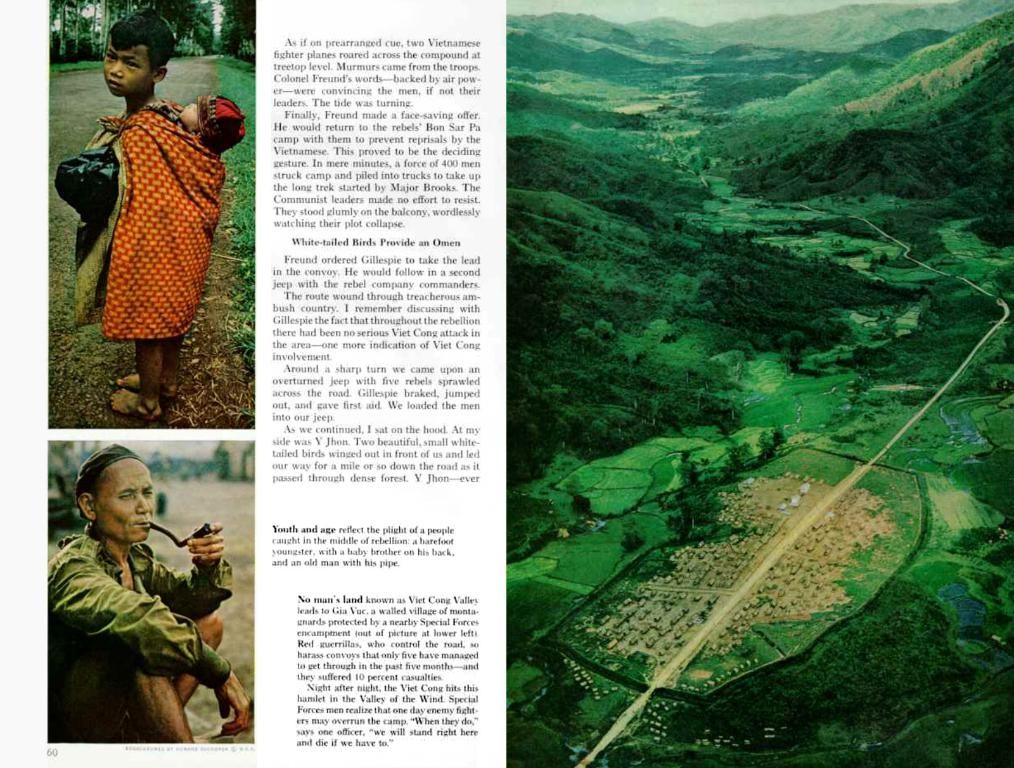
Experiencing chronic conditions, such as cardiovascular, respiratory, metabolic, and mental health issues, increases the risk of AFib, making it crucial to address these coexisting conditions.
A recent review highlighted various lifestyle factors, comorbid conditions, and socioeconomic factors that may influence AFib. An analysis of these insights emphasizes the need for multidisciplinary, individualized care to manage AFib effectively and reduce the risk of death and other health conditions.
Dr. Stephen Tang, a board-certified cardiac electrophysiologist, explains, "Comprehensive management of AFib goes beyond oral anticoagulation for stroke prevention or rate or rhythm control with medication or ablation. This complex disease is driven by numerous risk factors and comorbidities." He continues, "Identifying and optimizing these risk factors is essential in the management and control of AFib long term."
Genetic factors, sex, and increased age are nonmodifiable risk factors for AFib. Other risk factors for AFib include lifestyle factors, comorbid conditions, and socioeconomic factors. Blood thinners, or anticoagulants, can help manage AFib by reducing the risk of blood clot formation and stroke. Drugs like warfarin and newer nonvitamin K antagonist oral anticoagulants (NOACs) are typically used for AFib treatment.
Physical activity, weight management, and avoiding smoking and excessive alcohol consumption are essential lifestyle modifications for AFib prevention and management. Weight loss, particularly, is crucial as obesity is a significant risk factor for AFib development, as well as recurrence and complications like stroke and death.
Chronic cardiovascular, respiratory, and mental health conditions can increase the risk of AFib complications. For example, obstructive sleep apnea is associated with an increased risk of AFib recurrence post-catheter ablation and a higher chance of stroke.
The management and treatment of comorbid cardiovascular conditions, such as hypertension, help reduce the risk of AFib recurrence or complications like stroke. Anticoagulant therapy or catheter ablation is vital for reducing the risk of AFib-related complications, especially stroke.
Achieving better control of blood sugar levels and reducing weight can reduce the risk of AFib for individuals with diabetes. However, the association between high cholesterol, low-density lipoprotein levels, and AFib is less clear. Instead, higher triglyceride levels are associated with an increased AFib risk.
Kidney function is another factor that affects AFib management. Approximately half of all individuals with AFib exhibit impaired renal function, which can impact the metabolism of anticoagulant drugs and increase the risk of adverse effects.
Respiratory conditions, such as COPD, and short-term exposure to air pollution are linked to an increased risk of AFib. Some medications for COPD, like corticosteroids and theophylline, do not have adverse effects on individuals with AFib.
Psychological factors, such as stress and depression, are associated with a higher AFib risk. Depression is also connected to a heightened risk of AFib complications. Yet, the connection between cognitive impairment and dementia and AFib requires further research.
Overall, since the risk of AFib varies for each person, a multidisciplinary approach tailored to a specific patient is needed. A team of healthcare professionals can help manage various factors affecting AFib, offering the best treatment options and increasing the chances of favorable outcomes.
If you're living with AFib, speak with your doctor about managing your condition, especially if you have other chronic conditions. Adopting healthy lifestyle choices and working closely with your healthcare team will help manage and reduce the impact of AFib on your life.
- Obesity, alongside other factors like physical activity, diabetes, and smoking, contributes to the development and management of Atrial Fibrillation (AFib).
- Scientific insights suggest the need for a predictive approach in managing AFib, focusing on lifestyle factors, comorbid conditions, and socioeconomic factors.
- AFib is associated with a higher risk of chronic diseases such as stroke, heart disease, and depression, thus making it crucial to address coexisting conditions.
- The management of AFib extends beyond medication and ablation, requiring a holistic approach that addresses numerous risk factors and comorbidities.
- Nutrition, fitness, and exercise play a significant role in AFib prevention and management, particularly weight loss for those with obesity, a significant risk factor for AFib.
- Mental health conditions like stress and depression increase the risk of developing AFib and complications associated with it.
- Financial resources are significant in accessing the best care and treatments for AFib, as well as managing the conditions that contribute to it, such as diabetes.
- Career opportunities in the medical field, such as education and self-development, can lead to advancements in understanding and managing AFib, benefiting public health and wellness.
- Respiratory conditions like COPD and short-term air pollution exposure are linked to an increased risk of AFib, but some medications for COPD have no adverse effects in individuals with AFib.
- Individualized care tailored to specific patients is vital for AFib management, with healthcare professionals collaborating to address various factors affecting the disease, ultimately increasing chances of favorable outcomes.